People at risk for Alzheimer’s disease who do more moderate-intensity physical activity, but not light-intensity physical activity, are more likely to have healthy patterns of glucose metabolism in their brain, according to a new UW-Madison study.
Results of the research were published today online in Journal of Alzheimer’s Disease. Senior author Dr. Ozioma Okonkwo, assistant professor of medicine, is a researcher at the Wisconsin Alzheimer’s Disease Research Centern and the Wisconsin Alzheimer’s Institute at the UW School of Medicine and Public Health. First author Ryan Dougherty is a graduate student studying under the direction of Dr. Dane B. Cook, professor of kinesiology and a co-author of the study, and Dr. Okonkwo. The research involved 93 members of the Wisconsin Registry for Alzheimer’s Preventionn (WRAP), which with more than 1,500 registrants is the largest parental history Alzheimer’s risk study group in the world.
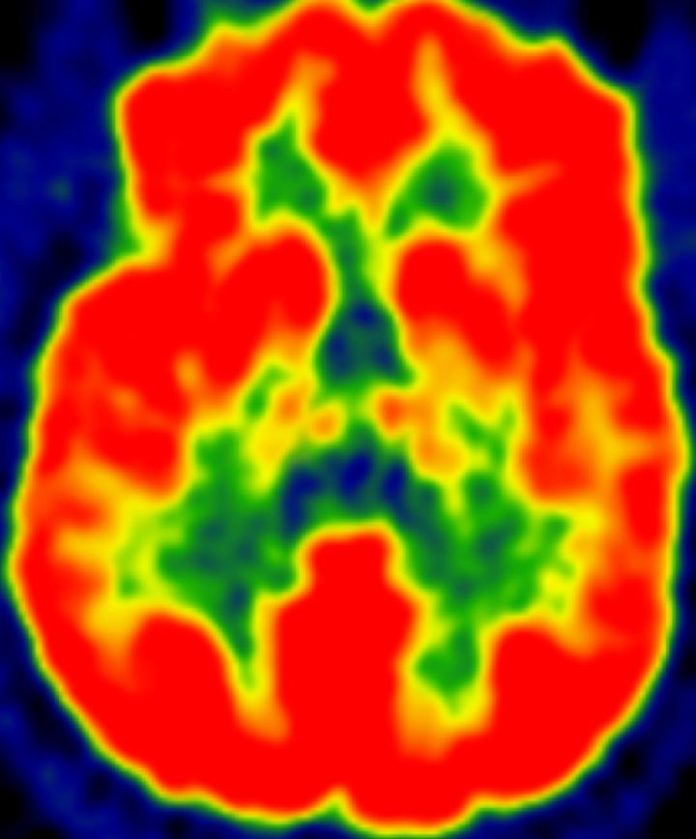
Researchers used accelerometers to measure the daily physical activity of participants, all of whom are in late middle-age and at high genetic risk for Alzheimer’s disease, but presently show no cognitive impairment. Activity levels were measured for one week, quantified, and analyzed. This approach allowed scientists to determine the amount of time each subject spent engaged in light, moderate, and vigorous levels of physical activity. Light physical activity is equivalent to walking slowly, while moderate is equivalent to a brisk walk and vigorous a strenuous run. Data on the intensities of physical activity were then statistically analyzed to determine how they corresponded with glucose metabolism–a measure of neuronal health and activity–in areas of the brain known to have depressed glucose metabolism in people with Alzheimer’s disease. To measure brain glucose metabolism, researchers used a specialized imaging technique called 18F-fluorodeoxyglucose positron emission tomography (FDG-PET).
Moderate physical activity was associated with healthier (greater levels of) glucose metabolism in all brain regions analyzed. Researchers noted a step-wise benefit: subjects who spent at least 68 minutes per day engaged in moderate physical activity showed better glucose metabolism profiles than those who spent less time.
“This study has implications for guidingn exercise ‘prescriptions’ that could help protect the brain from Alzheimer’s disease,” said Dougherty. “While many people become discouraged about Alzheimer’s disease because they feel there’s little they can do to protect against it, these results suggest that engaging in moderate physical activity may slow down the progression of the disease.”